Table of Contents
In this series of articles, NIZO Food Research Division Manager and FoodNavigator advisory panel member René Floris discusses some of the big issues in today’s food industry.
The consumer desire for immune health benefits from food products has received a boost from the ongoing Covid-19 pandemic, offering food manufacturers additional opportunities to add new value to their products. Alwine Kardinaal, Expertise Group Leader Nutrition & Health at NIZO, explains how in vitro and clinical testing can help manufacturers select and produce the best ingredients for supporting and maintaining better immune health.
René Floris: What is the relationship between food and the immune system?
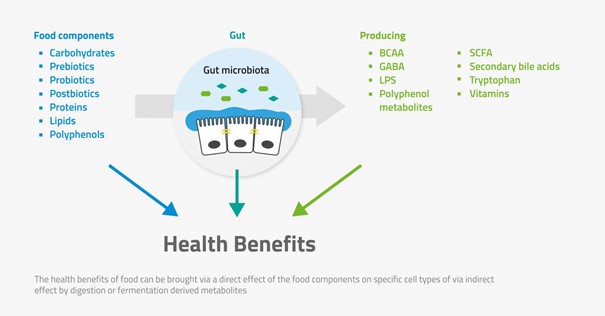
Alwine Kardinaal: We’ve long known that a healthy lifestyle is important to maintaining a strong immune system: no smoking, regular exercise, healthy body weight, etc. But there are also ingredients or components that have been shown to play a role in supporting the immune system, when ingested. These include specific vitamins and minerals, such as copper, iron, folate, selenium, zinc, vitamins A, B6, B12, C and D, as well as compounds including omega-3 fatty acids, polyphenols and certain milk ingredients. Then there are pro- and pre-biotics, yeast beta glucans, human milk oligosaccharides, pectins, etc., that can have an immune effect specifically via the gut microbiota.
In addition to occurring naturally in a food, these elements may be added by food producers into their products, in order to provide an immune health benefit. But it isn’t a question of simply adding an ingredient or compound. Firstly, you need evidence that the component does indeed provide the benefit. Then you want to be sure you are selecting the ingredient with the best potential for your product.
RF: What is the link between the gut and the immune system, specifically our response to infections or pathogens?
AK: The human immune system is very complex, involving the interaction of many cells and tissues in the body. It has two distinct parts that work closely together: the innate immune system regulates the body’s short-term response to an external invader, while the adaptive immune system ‘memorises’ the response and regulates the long-term reaction.
Gut health is strongly linked to the immune system, although it is only one aspect of this complex network. The gut is the first point of contact between the components and the body. Furthermore, the gut walls comprise a huge number of immune cells – around 70% of our total immune cells. However, the number of cells isn’t as important as their ability to respond to an external challenge, such as an infection. This is both in terms of the first reaction to pathogenic invaders such as bacteria and viruses, and then the enhanced reaction in the event of a re-infection – has the adaptive immune system done its job?
RF: How can food manufacturers gain a greater understanding of how a food ingredient interacts with the immune system?
AK: Ideally, you want to understand the ‘how, why and what’ of an ingredient’s immune health effect. Not simply if it has an immune effect, but specifically what that effect is, and its mechanism of action. An integrative approach can help in this understanding, including pre-clinical and clinical trials, combined with expert interpretation.
In order to evaluate the impact of the ingredient or component, you need to look at changes to the immune system after ingestion. The types of changes you see will give you an idea about the mechanism of action. However, as clinical trials can be costly and take time, starting with in vitro tests can be a fast and cost-effective way of gaining insight, especially if you don’t yet have a lot of information about the ingredient. Using expert interpretation, you can then design a focussed clinical trial that is more likely to provide you with the evidence you need.
RF: What types of in vitro tests can be used to evaluate potential immune response?
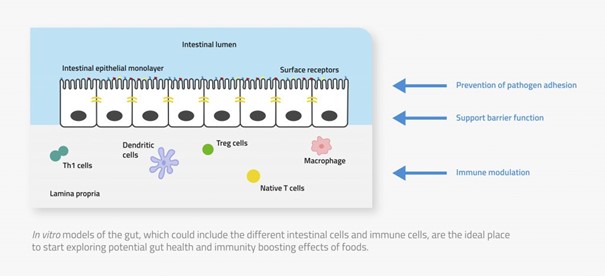
AK: You may need to combine multiple in vitro models to fully understand your ingredient’s impact on the immune system and the reactions in the gut.
Cell-based assays can be used to evaluate specific functionalities. Intestinal cells are exposed to pathogens, to determine whether the ingredient inhibits the pathogen from binding to the gut wall, affects the immune cell function, or stimulates the production of anti-inflammatory compounds, for example.
But the gut is a very complex environment. Combining these assays with in vitro digestion models lets you see what happens to the ingredient and its potential immune benefits once it has been fermented in the colon, or has come into contact with the beneficial metabolites produced by the gut microbiota, etc.
RF: What information are we looking for from the clinical trials?
AK: While the in vitro tests can give us insight, you can only determine the actual impact of the ingredient by seeing it in action, in the real body.
A human clinical trial on immune health benefits is intended to provide scientific evidence of whether the food component impacts resistance to infection. This can either be reducing the likelihood of getting ill, or decreasing the severity of the disease or of the symptoms.
RF: What role does the design of the clinical trial play?
AK: There are different types of clinical trials to choose from: the best design can depend on the ingredient’s mechanism of action, whether it impacts the innate or adaptive immune system, and more. For example, in vaccination trials, healthy volunteers are given either the active ingredient or a placebo, and then they are vaccinated, after which you measure antibody response. This is a measurement of the adaptive immune system – but if your ingredient acts instead on the innate immune system, you won’t get the results you need.
Perhaps an infection study would be better: exposing healthy volunteers to an attenuated form of the E. coli strain that causes traveller’s diarrhoea, for example, and then monitoring symptoms and other health measurements over time. Expert interpretation of the in vitro findings can help make sure you use the right clinical design the first time.
RF: Why is it important to include isolation and food processing techniques in the testing?
AK: The bioactive compound you want to use may be hidden in a larger structure, but you need to take care in how you isolate it: you could end up with different structures and biological effects. The same holds true for processing: heat and other treatment can damage the immune-active structure of your component.
Beta glucans from yeast and fungi, for example, are very promising for immune health benefits. However, the isolation and manufacturing methods used can change the structures, resulting in altered, or even no, immune effects. By testing this already at the in vitro stage, you don’t run the risk of completing your preclinical and clinical trials, only to discover your chosen ingredient won’t work with your processing conditions.
In our next column, we will discuss ‘Cereus business: preventing toxin production in foods’
Related cases
Related blogs
© NIZO 2025 | Sitemap - Privacy Statement - Cookie Statement - Terms & Conditions
Website by: Online Marketing Agency